ROSA® Knee robotic technology is designed to work with your individual anatomy. ROSA, which stands for Robotic Surgical Assistant, is designed to help your specially trained surgeon tailor the placement of your knee implant just for you.
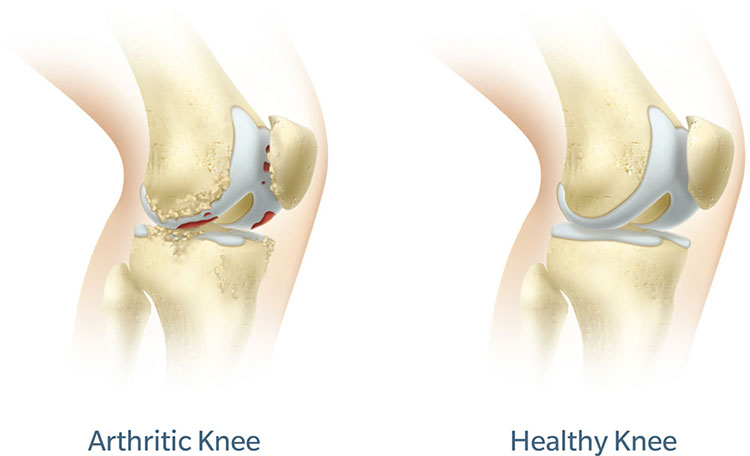
Arthritis in the Knee Joint
The knee is a hinge joint formed by the tibia (shinbone), femur (thighbone) and patella (kneecap). The ends of the bones in the knee joint are covered with cartilage, a tough, lubricating tissue that helps cushion the bones during movement.
Osteoarthritis, the most common form of arthritis, is a wear-and-tear condition that destroys joint cartilage and bone. It typically develops after years of constant motion and pressure in the joints. As the cartilage continues to wear away, the joint becomes increasingly painful and difficult to move. If conservative treatment options fail to provide relief, your surgeon may recommend total knee replacement using ROSA Knee robotic technology.
ROSA Knee Robotic Technology
 Getting a precise knee implant fit is important to your comfort and overall experience following knee replacement surgery. ROSA Knee robotic technology uses data collected before and during surgery to inform your surgeon of many details related to your unique anatomy that may affect your implant fit. By using this data to make more informed decisions, your surgeon is able to plan for and carry out a personalised surgery based upon your individual needs.
Getting a precise knee implant fit is important to your comfort and overall experience following knee replacement surgery. ROSA Knee robotic technology uses data collected before and during surgery to inform your surgeon of many details related to your unique anatomy that may affect your implant fit. By using this data to make more informed decisions, your surgeon is able to plan for and carry out a personalised surgery based upon your individual needs.
Before surgery
Your preoperative experience will be like that of most total knee patients. But, unlike traditional knee replacement methods, with ROSA Knee robotic technology, a series of x-rays may be used to create a three-dimensional (3D) model of your knee anatomy. This 3D model will enable the surgeon to plan many specifics of your knee replacement prior to your surgery.
During surgery
The surgical procedure using ROSA Knee robotic technology is similar to traditional total knee replacement, but with a robotic assistant. Your surgeon has been specially trained to use ROSA Knee in order to personalise the surgical approach for your unique anatomy. It’s important to understand that the robot does not operate on its own. That means it does not move unless your surgeon prompts it to. Your surgeon is still in the operating room the entire time and is making all of the decisions throughout your surgery.
During your procedure, ROSA Knee utilises a camera and optical trackers attached to your leg to know exactly where your knee is in space. Think of it like a very detailed global positioning system (GPS) that you might use in your car. If your leg moves even a fraction of an inch, the robot can tell and adjusts accordingly. This helps ensure that the plan your surgeon put into place is executed as intended. Throughout your surgery, ROSA Knee provides your surgeon with data about your knee. This information, combined with your surgeon’s skill, helps them know how to position your implant based on your unique anatomy.
After surgery
Following surgery, you will be hospitalised based upon the recovery plan your surgeon decides is best for you. This hospitalisation may range from one to three days. Recovery time varies, but most people should be able to drive after two weeks, garden after three to four weeks, and golf after six to eight weeks. Your surgeon will tell you when and what activities you can return to, and what activities to avoid.
Complications
While uncommon, complications can occur during and after surgery. Some complications include, but are not limited to, infection, blood clots, implant breakage, malalignment and premature wear, any of which can require additional surgery. Although implant surgery is extremely successful in most cases, some patients still experience stiffness and pain. No implant will last forever, and factors such as your post-surgery activities and weight can affect longevity. Be sure to discuss these and other risks with your surgeon.
There are many things that your surgeon may do to minimise the potential for complications. Your surgeon may have you see a medical physician before surgery to obtain tests. You may also need to have your dental work up-to-date and may be shown how to prepare your home to avoid falls.